Meet the Carousing, Harmonica-Playing Texan Who Won a Nobel for his Cancer Breakthrough
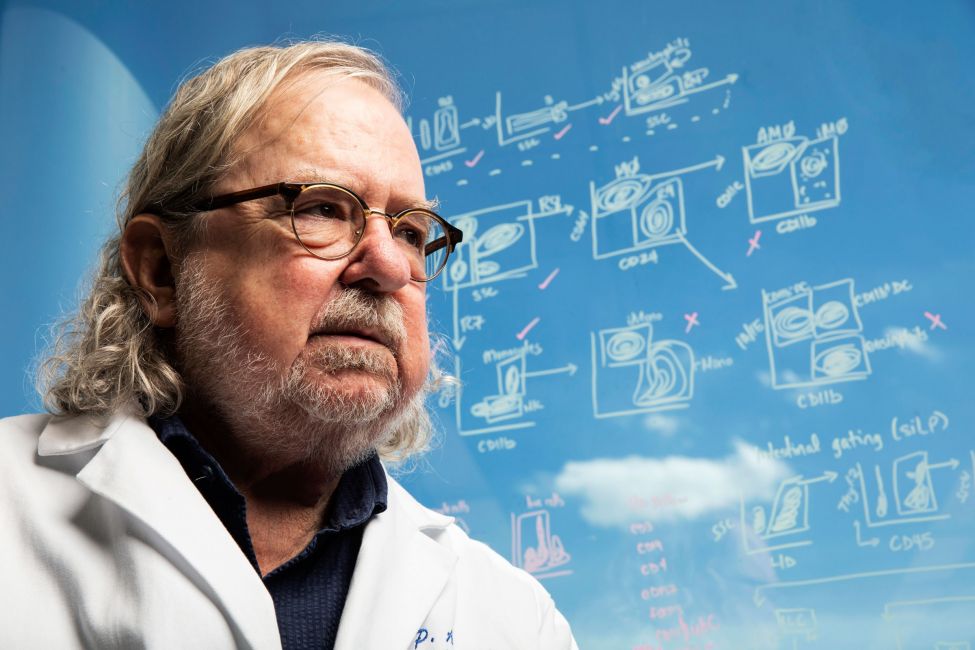 Jim Allison is an iconoclastic scientist who toiled in obscurity for years. Then he helped crack a mystery that may save millions of lives: Why doesn’t the immune system attack cancer? Chance favors the prepared mind. —Louis Pasteur WIRED magazine on 10.22.2018 JAMES ALLISON LOOKS like a cross between Jerry Garcia and Ben Franklin, and he’s a bit of both, an iconoclastic scientist and musician known for good times and great achievements. He also doesn’t always answer his phone, especially when the call arrives at 5 am, from an unfamiliar number. So when the Nobel Prize committee tried to reach Allison a few weeks ago to inform him he’d been awarded the 2018 Nobel Prize in medicine, Allison ignored the call. Finally, at 5:30 am, Allison’s son dialed in on a familiar number to deliver the news. The calls have not stopped since.
These “cut, burn, and poison” techniques are currently estimated to be able to cure cancer in about half of the people who develop the disease. And that’s remarkable, a true medical accomplishment. But that leaves the other half of cancer patients. Last year, in the United States alone, that translated to nearly 600,000 people who died of the disease. The fight was never fair. We’ve been pitting simple drugs against creative, mutating versions of our own cells, trying to kill the bad ones while sparing the good ones, and making ourselves sick in the process. And we’ve been doing that for a very long time. But now we have added a new and very different approach—one that doesn’t act directly on cancer, but rather acts on the immune system. And that’s the breakthrough. THE IMMUNE SYSTEM has evolved over 500 million years into a personalized and highly effective natural defense against disease. It is a complex biology with a seemingly simple mission: to find and destroy anything that’s not supposed to be in our bodies. Hundreds of millions of immune cells circulate throughout the body, searching out and destroying invaders that make us sick and body cells that have become infected, have mutated, or have become defective—cells like cancer. Which raises the question: Why doesn’t the immune system fight cancer already, the way it fights even the common cold? For more than 100 years, medical researchers puzzled over that question. Most concluded that the immune system and cancer simply had nothing to say to each other. The argument was that since cancer is a normal body cell gone rogue, it is too much a part of us to ever trigger an immune response. Cancer immunotherapy was condemned as a quaint if simplistic idea based on high hopes and bad science. But despite the mounting mockery of the larger scientific community and dwindling research funds, a handful of immunotherapy researchers continued to believe—and continued searching, decade after decade, for the missing piece of the cancer immunity puzzle, a factor that prevented the immune system from recognizing and attacking cancer cells. The stakes could not have been higher. If such a missing piece could be found, it would radically reshape our scientific understanding of both ourselves and disease and possibly revolutionize medicine on a scale not seen since the invention of vaccines. It might allow us to finally unleash our immune system, enabling it to recognize and attack cancer the way it does other diseases. It might even pave a new road to the cure. For the tens of millions more diagnosed with cancer each year, the race to find the missing piece of the cancer-immunity puzzle was literally a matter of life and death. But despite the occasional glimmer in the darkness, generations of researchers had tried and failed to find this missing factor. Nobody could even say for certain that such a such a piece existed. And certainly nobody would have guessed that it would be discovered by a hard-living, harmonica-playing Texan who hadn’t even been looking for it. THE STRETCH BETWEEN 1965 and 1973 were peak years if you were young and musical in Austin, when the little university town was just beginning its metamorphosis into the tech and freak capital of a cowboy state—Texas enough to two-step, hippie enough to do it stoned, and smart enough to work the newly relocated tech mills of Texas Instruments, Motorola, and IBM. Jim Allison fit right in.  Allison initially thought he would go to medical school but soon realized he was more interested in research and set out to earn a PhD in biochemistry. COURTESY OF JIM ALLISON
He had outgrown his hometown of Alice, Texas, when the local high school failed to offer an advanced biology class that dared mention Charles Darwin. He turned to correspondence courses from the University of Texas at Austin. and after graduation he enrolled full-time, a 17-year-old bound to be a country doctor like his dad. Back then, the 2018 Nobel Prize in medicine wasn’t even a twinkle in the young Texan’s eye.
In the experiment, once the enzyme eventually robbed the tumor of all its fuel, the tumor went necrotic and “disappeared.” Allison wanted to know where it went. Allison says. His curiosity led him to his first glimpse of a biology he would eventually redefine, and the first tenuous steps toward a generational breakthrough in the war against cancer. Allison knew the disease intimately. He’d been just a kid when he lost his mom to it, had held her hand as she went, not even knowing what the disease was or why she had burns, only knowing she was gone. He’d lose most of his family that way eventually, and though he’d never say it out loud, and wouldn’t even much voice it to himself, in the back of his mind killing cancer would always be the one potential, practical outcome of his otherwise pure scientific research. Allison would follow his curiosity like a north star, wandering for decades, but heading home all the while. The dead tumors in his mouse cages hadn’t just disappeared by magic, of course—it was biology. The human body sheds old, dead cells (a mass roughly equal to our body weight each year) the way trees shed leaves, and for essentially the same reason. The process (called “apoptosis,” from the Greek for “to fall away”) allows fresh daughter cells to take their place. The spring cleaning is carried out by hungry, blobby Pac-Man cells in our blood—part of a 500 million-year-old personal defense force that Allison’s textbooks called the innate immune system. Today, aspects of our immune system still remain a mystery, but when Allison began his studies it hadn’t really even been explored, a sort of deep-ocean ecosystem in the human body. “New” aspects of the immune system, like the hunter-killer T-cells, were barely on the radar yet (Allison’ s college professor thought they were “too weird” evolutionarily to really exist). But some of the older aspects of the defenses in our bloodstream had been worked out, especially those of the innate immune system, which works much the same in sea sponges as it does in humans. The ancient players of the innate immune system are charismatic and deceptively straightforward. They also happen to be big enough to be seen wiggling and eating under the microscope. That includes amoeba-like cells adept at squeezing between body cells and patrolling our perimeter (inside and out, we have a surface larger than a doubles tennis court), looking for what shouldn’t be there and killing it. Some of the innate immune cells are small, blobby smart patrollers called dendritic cells. Others are similar-looking but larger blobby characters called macrophages (literally, “big eaters”). Most of what they eat are those retired body cells—normal cells that have hit their expiration date and politely self-destructed, through apoptosis. They also eat bad guys. Macrophages have an innate ability to recognize simple invaders. Most are the usual suspects of disease—the bacteria, fungi, parasites, and viruses that evolved right alongside us for millennia. These foreign, or “non-self,” cells are recognizable as foreign because they look different—that is, the fingerprint of chemical arrangements of proteins on their surfaces is different. Macrophages look for anything they recognize as foreign, then grab and gobble it. Casablanca. Good guys, bad guys, reporters and soldiers, macrophages, dendritic cells, T and B cells, and even diseased cells, everyone goes to Rick’s.) The information triggered other cells in the adaptive immune system to ramp up into a massive clone army in specific response. Allison knew that was basically how vaccines worked—by presenting the body with dead samples of a disease that it might encounter later. This introduction triggers the immune system to build up forces against anything that looks like that sample. Then later, if the live disease does show up, an immune army will be waiting for it. Now, Allison wondered if something like that was happening in his mouse cages, too He’d killed the tumor. The mouse macrophages were gobbling up the mutant cells and clearing them out. In the process, they were surely carrying back those distinctive mutant proteins and showing them to the killer cells of the adaptive immune system. And wasn’t that sorta how a vaccine worked? So, Allison wondered, did that mean his experiment had, in a roundabout way, vaccinated his mice against this specific form of blood cancer? Were they now “immune” to this cancer? “Just for the hell of it, I was setting up another experiment, and I decided that since I had these mice that were cured—who were just sitting there, eating—I would inject them with the tumor again, but not treat them with the enzyme this time, and see what happened,” Allison remembers. He hadn’t asked permission, he didn’t write a protocol, nothing. He simply shot from the hip. And what happened was ... nothing. “They didn’t get tumors,” Allison says. “I went back and injected them with 10 times as much, and they still didn’t get tumors. I injected them with another five times more, and they still didn’t get tumors! Something was happening here,” Allison says. “Something amazing!”  “It was great,” Allison says of his time as a researcher at MD Anderson Cancer Center outside of Houston. “The camaraderie—nobody expected any payback for anything. They did it because it's what you did, you know? It was heaven.” THE UNIVERSITY OF TEXAS MD ANDERSON CANCER CENTER/COURTESY OF JIM ALLISON As a casual one-off, the experiment hadn’t really proved anything. (“People talked about doing it in humans, you know, just taking your own tumor and mashing it up somehow and injecting it back, but it doesn’t really work that easily.”) But it had provided Allison his first glimpse of the mystery and potential of the immune system and its most recently discovered component, the T cell. His professor was only half wrong—they did exist, but they were, in fact, weird. Good weird, Allison thought. They were killers, some of them, but there were other types that “helped” complex immune responses, making it possible to somehow be prepared to recognize and kill diseases that the human body had never encountered before. And, really, there was no telling how much we didn’t yet know. Simply put, this was the most interesting thing Jim Allison had ever come across. So he decided to switch tracks, again, and study that. BY 1973, AFTER eight years spent getting his BA, MS, and PhD in Austin, Allison wanted to stretch his legs and find somewhere new and “first-rate” for his immunology research, and that took him 1,300 miles west into California and a postdoc program at the prestigious Scripps Institute. He was married now, doing lab work by day and playing harmonica with a country-western band a couple nights a week. “Our band got pretty famous in what was called the North County,” Allison says. “People think it’s all like LA or something, but that part of California’s pretty redneck.” Fights were brief but frequent. “Usually, it'd start because one cowboy that's doing a two-step would swing too widely and bump into a guy, and the guy would say, ‘Don't do that again.’ But, that's just the way the guy danced, you know? He danced big. So it happened again. Pretty soon there’s beer and fists everywhere.” Allison was the only one in the band with a day job, but playing with full-time musicians put him quickly into the local music scene. Plus, Allison was the guy with the VW microbus. “So we’d go to these parties. There was one up the road in Del Mar—we walk in, I don’t know anyone. It was a pretty magnificent party by the way,” Allison says, “with Waylon Jennings and Tammy Wynette doing a few songs each, then Willie Nelson—turns out it was a celebration of his Red-Headed Stranger album.” The two Texans got to talking and partying, and next thing Allison’s got Willie and some of his band in the back of the microbus, on the way to open-mic night at the Stingray. “Man, they sold a lot of beer that night,” Allison says. Willie had taken the mic, asking, “You all mind if I stand in and play a few?” then played for four hours. “I never had to pay for another one in that bar again,” Allison says. Afterward he took the band back to the hotel. “Yeah, that was good,” Allison says. “And somehow we managed to avoid getting arrested.” Meanwhile, Scripps wasn’t really working out the way he’d imagined. “I was purifying proteins and sequencing them and all this stuff, working on the key molecules of the immune system,” he says, “but it really wasn't immunology.” Allison was interested in systems. “But we were discouraged from what the older guys called, you know, ‘model building.’ Like, ‘Don't build models, just do your work. Don't think.’ Yeah. It was very frustrating. I figured, if this is what science is, I don’t like it.” The cutting edge of cancer therapy might look very different had Allison quit the field right there. Instead, he went home and got lucky. Back in Texas, the MD Anderson Cancer Center was opening a new outpost lab near the town of Smithville. “Yeah, it was pretty weird.” Allison says. “Some economic stimulus thing from the governor, on donated land and with state money. And it was in the middle of an 18-acre state park. They’d just set up some lab buildings and hired six faculty members to go out there.” The idea was to fund a team to study carcinogenesis—how cancer starts. But in reality, Allison soon discovered, they pretty much had free reign. “Yeah, that was the weird thing at the time, because after they started this thing, the MD Anderson president changed. The new guy came in and said, "What do you do? What the hell is that?" You know? So they kind of just forgot about us and pretty much left us alone.” This was Allison’s kind of place. His colleagues were bright, enthusiastic scientists his own age—the oldest were in their thirties—who worked late, helped each other with their experiments, kept beer in the lab for ones that ran overnight, and pooled intellectual resources without ego or credit getting in the way. “It was great,” Allison says. “The camaraderie—nobody expected any payback for anything. They did it because it's what you did, you know? It was heaven.” The setup was sweetened by a total lack of teaching or administrative responsibilities, a Norton Commando 850 motorcycle, and enough NIH and NCI grant money to pursue what Allison was really interested in—the T cell. “It was a fantastic time in science because immunology had just been this poorly understood field,” he says. “I mean, everybody knew we had an immune system, because there were vaccines. But nobody knew much about the details of anything.” One of the things nobody knew was how a T cell recognized a sick cell in the first place. By now it was understood that T cells killed off normal body cells that had become sick or infected. But exactly how a T cell “saw” that sick body cell, how it recognized the distinctively foreign sick cell proteins (or “antigens”) on the cell’s surface, was still a stone-cold mystery. Allison read every academic paper he could find on the topic, then read the papers cited in them. There were plenty of theories about how a T cell recognized antigens. Most assumed that each T cell had a unique type of receptor (a specific arrangement of proteins extending from the cell surface) that recognized a specific antigen expressed by a sick cell, homing in and fitting something like a key into a lock. That was a reasonable theory, but nobody had actually found one of the receptors. If they existed, there should be a lot of them, scattered among all the yet-uncounted proteins that stuck out from the T-cell surface (there are so many that new ones are given numbers, like newly identified stars). Those “receptor” proteins would be molecules built in some sort of double-chain-like configuration. Several labs were convinced that it would look just like it did on another denizen of the adaptive immune system that “sees” antigens, the B cells. Which, Allison thought, was stupid. “People from Harvard and Johns Hopkins and Yale and from Stanford were already claiming they had a molecule that was the T cell receptor,” Allison says. “Most of them, because B cells make antibodies, figured that in T cells the receptor had to be an antibody-like thing, too.” Whatever it looked like, if you could find it, in theory you could manipulate it. Control the T-cell receptor and you might control what the immune system’s killing machine targeted. The result could have massive implications for humanity, and a massive name—and maybe even a Nobel Prize—for whoever found it. B CELLS AND T cells are both part of the adaptive immune system. They look so similar that they cannot be distinguished under an optical microscope—part of the reason they’d gone undiscovered for so long. But B and T cells would turn out to be distinct types of immune cells, which see and attack foreign or non-self cells in very distinct ways. Allison didn’t believe that T cells were just a cell-killing version of B cells, a sort of killer-B. He believed that if T cells existed (they did) and were different from B cells (they were), then those differences were the point. The T cell wasn’t just more of the same—it was a unique cell type that did a unique job, and accomplished it in a unique way, through a unique biology.  The race to clone the T-cell receptor protein gene was intense. "I mean, everybody realized there was a Nobel Prize at the end of it," Allison says. "Everybody was scrambling, man.” SCOTT DALTON “We didn't have a library to speak of in Smithville,” Allison remembers, but he had access to an excellent library down the road, thanks to having finagled an adjunct appointment with the main MD Anderson campus in Houston and a newly restored ’54 Mercedes for the back-and-forth. “I'd go and Xerox big stacks of shit and then read it,” he says. He was looking to better understand the T cell receptor. But what Allison was reading in the academic journals didn’t really make sense to him. “Yeah, when that happens, the fact that it doesn't make sense is either their fault or your fault,” Allison laughs. Naturally, his first assumption was that it was his fault. “I'd think, ‘I'm an idiot. I can't understand this.’” Allison says. “Then, I thought, ‘No, they're idiots. They don't understand what they're talking about!’” Then he’d drive back out to the library and copy another stack. All the reading and wondering came together one night while Allison was in Houston sitting in on a lecture by a visiting Ivy League immune researcher. Something just clicked. “I said, 'I think I know a shortcut to finding the T-Cell receptor.'" Suddenly it seemed so obvious: If Allison could rig up a way to compare B cells and T cells, devise a lab experiment that put one against the other and let their redundant surface proteins cancel each other out, the receptor should be the molecule that didn’t cancel out. Essentially, he was looking for a needle in a haystack, and his idea was to set fire to the haystack and sift the ashes—or as Allison puts it, “pick it out of the weeds.” Whatever was left would be the needle he was looking for. He gunned the Merc back to the Smithville lab and got to work. The idea was relatively simple, but the steps were numerous, and Allison had to make all the assays himself, which was tedious work. “The assays were so crude,” Allison says. “The end point involved holding a piece of film up and trying to guess which circle was bigger out of 100, you know? Then doing that with maybe 1,000 different films. People laughed at us. I’m really surprised that it worked.” And yet, it did work. “It was a success, the very first time,” he says. “So now I’ve got a thing that’s on T cells but not on B cells, not on any other cells— so, that’s gotta be the T-cell receptor!” He showed that the receptor was a two-chain structure—an alpha and a beta chain, and he wrote it up in a paper. Allison was hoping to be published by one of the leading peer-reviewed research journals. But nobody at Cell or Nature or any of the A-list, peer-reviewed journals was willing to publish the findings of this junior academic from Smithville, Texas. “Finally, I ended up publishing the results in a new journal called The Journal of Immunology.” It wasn’t Science or the New England Journal of Medicine, but it was in print, and in the world. “At the end of the paper, I said, ‘This might be the cell antigen receptor, and here are the reasons why I think that it is the T-cell antigen receptor,’ and I just listed it out, all the reasons.” It was a bold announcement regarding the biggest topic in immunology. “And nobody noticed it,” Allison says. “Except in one lab.” The Gordon meeting helped put the brash young scientist on the academic map and won him an appointment as a visiting professor at Stanford University. It also gave him license to pursue the next intellectual milestone. Now that the T-cell antigen receptor had been identified and its two-chain molecular structure had been described, the race was on for the greater prize: the blueprints for those proteins, as encoded in genes in the T-cell DNA. “At that point, people had just figured out how you could work with DNA and clone genes, so now, everybody was trying to clone this T-cell receptor protein gene,” Allison says. “It had been the holy grail of immunology for 20, 25 years, and nobody had solved it. There was this huge, ugly race for about three or four years. I mean, everybody realized there was a Nobel Prize at the end of it. Everybody was scrambling, man.” The experience provided a valuable lesson to the young immunologist. “I mean, it got ugly. Ugly. But I met some really good people there too, some fine people,” Allison says. “So I sorta learned who was who.” “It was kind of controversial because I hadn’t been at the big labs,” Allison says. “I hadn’t been at Harvard. I lacked the pedigree of most faculty at places like Berkeley.” Which was why it blew his mind two weeks later when Berkeley offered him a full-time job, covered by a healthy grant from the Howard Hughes Medical Institute. Allison would have a lab and postdoc salaries, and he could research whatever he wanted. He didn’t need to teach, and the money might last forever with no strings. His only obligation was to occasionally give a presentation on his progress. “Then when you came up for review, it was pretty bad,” Allison says. “They would have 50 of the top scientists in the world in the room. You would give a 25-minute talk, and it was 25 exactly. When minute 25 came, it was ‘Stop. Questions?’ It was really frightening. Literally, sometimes the night before I’d just be in the bathroom throwing up.” Much had been discovered about T cells in the decade since their discovery. Now it was widely accepted that there were different kinds of T cells, with different specialties for coordinating an immune response against disease. Some “helped” immune response by sending out chemical instructions, via cytokines, like a quarterback calling plays. Others, the killer T cells, killed infected cells one-on-one—usually by chemically instructing those cells to commit suicide. “We thought that the T-cell antigen receptor was the ignition switch,” Allison says. That was the natural assumption.
If keying the T-cell receptor with the corresponding antigen wasn’t the only signal needed to turn on a T cell, that meant there had to be another molecule, maybe several, required to activate the T cell, what’s known as “co-stimulation.” Maybe the T cell required two signals—like the two keys for a safe deposit box, or how, when starting a car you need to key the ignition and also press the gas pedal to make it go. But where was the T cell’s gas pedal? Three short years later, they found it, another molecule on the T-cell surface called CD28. (CD stands for “cluster of differentiation,” which is sort of like calling it “a thing that’s clearly different from the other similar things around it”.) and co-stimulating CD28 did start up the T cell, but when they did that in mice models, the T cell often just stalled out. It was as if they’d found the key to the ignition and the gas pedal, but a third signal was still necessary to make the T cell go. So now they went hunting for that. One of Allison’s postdoctoral students, Matthew “Max” Krummel, compared the structure of the protein CD28 to other molecules, looking for something similar in a sort of computerized book of molecule mug shots—“the gene bank, that’s what we called it at the time,” Allison says. The idea was that if you found a molecule that looked similar, maybe it did similar things and was related, evolutionarily. Krummel soon found another molecule with a close family resemblance to the part of CD28 that stuck out of the cell, the receptor part. The molecule had recently been identified, named, and numbered. It was the fourth cytotoxic (cell-killer) T-immune cell (lymphocyte) identified in the batch, so Pierre Goldstein, the researcher who’d found it, called it cytotoxic T-lymphocyte-associated protein #4— or CTLA-4 for short. (A few decades later, these letters would be on the license plate of Allison’s convertible Porsche.)  Early on, Allison read every scientific paper he could find on T-cell receptors. “I'd think, ‘I'm an idiot. I can't understand this.’” he says. “Then, I thought, ‘No, they're idiots. They don't understand what they're talking about!’” THE UNIVERSITY OF TEXAS MD ANDERSON CANCER CENTER/COURTESY OF JIM ALLISON Meanwhile, researchers Jeffrey Ledbetter and Peter Linsley were working on the same third-signal problem at the Bristol-Myers Squibb research campus in Seattle. Finding the protein signal was one thing, but the point was understanding what it did. Blocking a signal (with an antibody that binds to it and basically prevents it from being used, like crazy-gluing a keyhole) and observing the result is a common method. “Linsley made an antibody to block CTLA-4,” Allison recalls. The group quickly published a paper, concluding that CTLA-4 was a third “go” signal, another gas pedal on the T cell that had to be activated for immune response. Having another researcher beat them to the anti-CTLA-4 antibody was disappointing. It was especially disheartening to Krummel, who had just spent three years working on the antibody as his intended thesis project. But Allison decided to proceed with more CTLA-4 experiments anyway. There was always more to learn—and besides, Allison wasn’t totally convinced that Linsley et al. had really solved the T-cell activation mystery. “I knew there were two ways you can get something to go faster,” Allison says. “One is to press on the gas pedal. The other is to take off the brake.” Allison says Linsley’s group had only devised experiments consistent with CTLA-4 being another “go” signal, essentially a second CD28. “I said, ‘Let’s do the experiments consistent with CTLA-4 giving an off signal.’ Sure enough, that’s what we found out. CTLA-4 was an off signal.” Jim Allison is a master of the Texas-sized understatement. Behind his simple statement of his lab’s new finding lies a discovery that has profoundly shifted our scientific understanding of how immunity works—and sometimes doesn’t—and how we can change those rules to turn the tables on cancer. ALLISON’S LAB NOW had a fairly complete picture of the steps required for T-cell activation against disease. The other two signals (CD28 and CTLA-4) were like the gas pedal and brake on the car. CTLA-4 was the brake—and it was the more powerful of the two. You could press both (and in experiments, Krummel found that was a crude way of controlling the activation rate), but if you floored both, the brake overruled the gas pedal and the T cell wouldn’t go, regardless of everything else. Or, more accurately, enough stimulation of CTLA-4 and immune response stalled out, regardless of how much the T cell was being triggered by a sick cell antigen. If all this sounds complicated, it’s because it is, on purpose. Allison’s lab had discovered an elaborate safety mechanism, an aspect of the larger framework of checks and balances that prevents the immune system from going into overdrive and attacking healthy body cells. Each safety is a sort of fuse that gets tripped if a trigger-happy T cell is programmed to target the wrong antigen, such as ones found on normal body cells. It was a way of repeatedly asking Are you sure about this? before T cells turned into killing machines. Proper triggering of immune response against pathogens is what keeps you healthy. However, pedal-to-the-metal immune response against healthy self cells is autoimmune disease. The double-check, double-signal mechanism of T-cell activation would turn out to be only one of many redundancies and fail-safe feedback loops built into immune response. Those “checkpoints” on T-cell activation hadn’t been guessed at before. But now Allison’s lab and, simultaneously, the lab of Jeff Bluestone at the University of Chicago had found one of those checkpoints. Bluestone was focused on ways of placing this new discovery in the context of organ transplants and diabetes, tamping down unwanted immune response. But Allison had a different idea where he’d like to stick it. Biology was interesting, diseases weird and fascinating, immunology cool. But cancer, Allison admits, “pissed me off” personally. Allison’s lab had always been dedicated primarily to pure immune research. But now Jim Allison had another experiment in mind, and an intellectual path to an emotional destination. As it happens, that road also eventually led to the Nobel Prize. ALLISON WROTE THE experiment out in late summer and gave it to his new postdoc, Dana Leach, who, he says, had “done some tumor stuff.” “I said, ‘I want you to give some mice tumors and then inject them with this CTLA-4-blocking antibody. Give other mice tumors but no anti-CTLA-4, and let’s see what happens.’” In November, Leach came back with the results: The mice that got anti-CTLA-4 had been cured of cancer. The tumors had disappeared. In the mice that didn’t have CTLA-4 blocked, the tumors kept growing. Allison was stunned—this wasn’t what experimental data looked like. “According to the data, it was a ‘perfect’ experiment, 100 percent alive versus 100 percent dead,” Allison says. “Jesus, I mean, I was expecting—something. But this was 100 percent. Either we’d just cured cancer or we’d really screwed up.” He needed to do it over again. “We had to,” Allison says. And they needed to start immediately—such experiments take a couple months. But it was Thanksgiving, and Leach wasn’t willing to give up his planned European trip over Christmas break, not for a bunch of mice. Allison told him to just set up the experiment again. “Right now, inject all the mice,” he said, “then go do whatever you’re going to do.” He told the postdoc to just label the cages A, B, C, and D. “I said, ‘I’ll measure the mice. Don’t tell me anything.’” Allison would do the grunt work and check the results for each cage, but until it was over, he wouldn’t know which group was which. “It was really harrowing,” Allison says. He’d come in every day and see that the tumors in cage A seemed to be getting bigger. He’d measure each tumor with calipers and mark the results on his gridded paper, then move to cage B and find the same thing, mice with growing tumors. Same story in cage C and cage D. There were a lot of mice, a lot of numbers, and they were all on the same track. It was 100 percent failure. Had his break-happy postdoc screwed up this experiment too? Allison felt he was moving backward. Finally, on Christmas Eve he was in the lab, staring at four cages of mice, all with steadily growing tumors. “I said, ‘Fuck—I’m not going to measure these anymore. I need to take a break from this.’” He hadn’t consciously known where he was going with all of this experimentation. Now, suddenly, they had arrived at a result and a biological mechanism. Maybe Allison and his lab had cured cancer in mice, one more time. Or perhaps they had just found a piece of the cancer immunity puzzle, one that might make sense of decades of confusing data. CTLA-4 was a safety checkpoint built into the body to help prevent the immune system from attacking the body or a developing fetus. Tumors survive and thrive, shielded by these built-in safety mechanisms on T cells, which effectively put the brakes on the body’s immune response against them. That was cancer’s survival trick, or one of them. At least, it was in mice. But if Allison could block it in mice, maybe he could block it in people. EUREKA! T cells could recognize cancer, but these inhibitory pathways stifle a complete T cell response, and you could block that. What else was possible? That question, and the hope it engendered—that was what mattered. And that was the breakthrough.
And, his wife says, Jim cries, every damn time. Adapted from the book THE BREAKTHROUGH: Immunotherapy and the Race to Cure Cancer. Copyright (c) 2018 by Charles Graeber. Reprinted by permission of Twelve/Hachette Book Group, New York, NY. All rights reserved. |
[premium_newsticker id="211406"]

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License