Introduction by Ritt Goldstein
Theory by Dr. Bernt Danielsson and Ritt Goldstein
Copyright November 2012

The water damage inside this apartment—typical of countless homes in the stricken area— almost guarantees the onset of mold, unless extreme remedial measures are taken immediately.
According to Wikipedia, “Katrina cough is a putative respiratory illness thought to be linked to exposure to mold and dust”. And, a new ‘illness’ has emerged in New York, Fox NY (and I never thought I’d cite Fox News) headlining “Far Rockaway Cough”, mold thought to play a role in it as well. But beyond coughing there are other symptoms that mold can cause, the US Centers for Disease Control (CDC) even having an advisory site for storm victims.
The CDC warns those affected by flooding that mold can be hazardous, so when deciding what belongings can be salvaged, they urge, “When in doubt, take it out!” As to how hazardous mold can be, the US Environmental Protection Agency (EPA) warns that some molds can produce mycotoxins, the EPA observing … Many symptoms and human health effects attributed to inhalation of mycotoxins have been reported including: mucous membrane irritation, skin rash, nausea, immune system suppression, acute or chronic liver damage, acute or chronic central nervous system damage, endocrine effects, and cancer. More studies are needed to get a clear picture of the health effects related to most mycotoxins. However, it is clearly prudent to avoid exposure to molds and mycotoxins.
Severe mold exposure can have significant and long-lasting health effects, some terming these effects ‘Sick Building Syndrome’. Several years ago, I and a colleague developed a theory on the physical mechanism through which such sufferers were affected, a theory we were invited to present at a Mold Symposium in Sweden’s parliament organized by the Swedish Green Party. The following is an article on the theory Dr. Bernt Danielsson and I developed, the below piece approximating the one we distributed at our Parliamentary presentation.
The theory is one which leans heavily upon Professor Beatrice Golomb’s work on Gulf War Illness, my readings of Golomb — coincidentally done in combination with readings upon research on the natural occurrence of chemical compounds called Acetylcholinesterase inhibitors in certain varieties of mold — leading me to contact Danielsson, spawning the work we did. However, Golomb’s theory provoked considerable controversy and debate, and today the actual causes of Gulf War Illnesses are yet debated. As for the mold theory Danielsson and I derived – while some medical scientists applauded it, it was never published in any journal, it remains untested. There is one certainty, however – the severity of illnesses which some of those having significant mold exposure are known to have experienced.
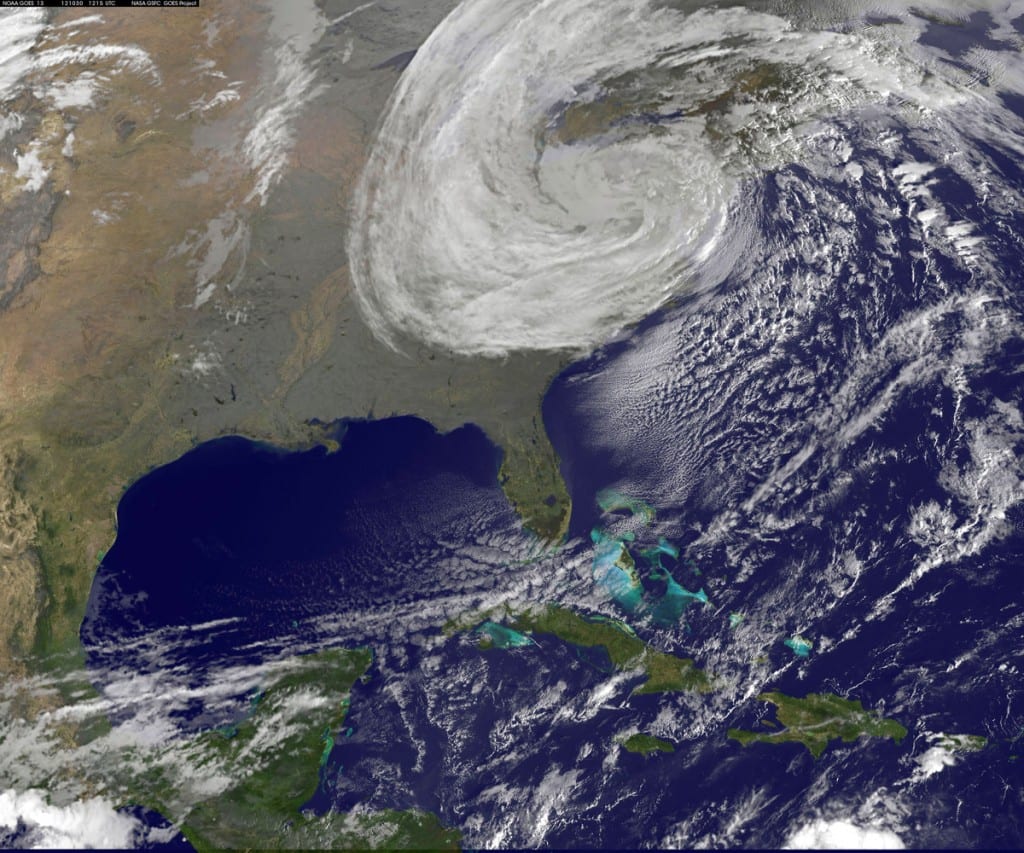
In view of Superstorm Sandy’s impact, it seemed time for the following to be made public.
SICK BUILDING SYNDROME AND GULF WAR ILLNESS – A COMMON CAUSE?
By Bernt Danielsson, MD, and Ritt Goldstein, UJ
A study linking the multisymptom problems of so-called Gulf War Illness (GWI) to acetylcholinesterase inhibitors (AChEis) was recently published: Professor Beatrice Golomb’s ’Acetylcholinesterase inhibitors and Gulf War illnesses’. In our following paper we hypothesize that AChEis are also connected to another, strikingly similar malady, but one vastly more widespread and affecting far larger numbers globally, particularly in The West – Sick Building Syndrome (SBS).
Since the 1970’s, debate has existed regarding the nature of so-called Sick Building Syndrome (SBS). More recently, similarities between SBS and GWI have fueled speculation as to the basis for such a commonality, a commonality that may now well be explained.
Spring 2008 saw the publication of Acetylcholinesterase inhibitors and Gulf War illnesses, Gulf War Illness (GWI) being the condition termed to describe the chronic symptoms endured by many veterans of the Gulf War (1990-91). Expanding upon the study’s conclusions of AChEi linkage to GWI, one might theorize that exposures to comparable levels of AChEis, in non-Gulf War settings, could potentially yield symptoms resembling those of GWI. Indeed, the study specifically states that its findings “may be relevant to a subset of civilians with chronic multisymptom complaints”,(1) opening a passageway to argue that AChEi rich mycotoxins, emanating from particular strains of indoor molds, may well be an unrealized cause of SBS. Having said this, we also believe AChEi linkage suggests that non-biological, chemical contaminants containing sufficient AChEi levels, could also yield SBS symptoms; though, we focus our attention upon mold.
Soma or Psyche?
Again, since the 1970´s debate has existed regarding the nature of SBS. As the pathophysiologic mechanism of SBS’s puzzling combination of symptoms has been hard to understand, the question of psychosomatic reaction has often been raised.
Paralleling the SBS experience, findings have shown that about 25 to 30 percent of Gulf War veterans suffer a set of chronic and equally puzzling symptoms.(1) As a result of these veteran’s symptoms, a very substantive amount of epidemiological, toxicological, and psychological research has sought both GWI’s cause and best treatment. Posttraumatic stress, burning oil wells, burnt-out uranium, nerve agents, and more have all been proposed as explanations of GWI’s cause.(1)
Given the lengthy GWI debate, the conclusions presented by Professor Golomb – that GWI resulted from AChEi exposure generally, and the use of pyridostigmine bromide as a nerve agent pretreatment particularly(1) – may be termed ’somewhat unexpected’ by some. However, beyond her study’s publication in one of America’s most respected scientific journals,(1) Golomb’s findings were confirmed by the US Department of Veterans Affairs’ Research Advisory Committee on Gulf War Veteran’s Illnesses – a body where the vast majority of members hold substantive scientific stature.
In a particularly telling observation, an observation upon what might be termed as a further similarity between GWI and SBS, the Committee pointedly observed that GWI had been ”poorly understood and, for too long, denied or trivialized”.(2)
However, regardless as to one’s position upon the relation of GWI to AChEis, Golomb’s study does note that there is a history of illness among agricultural workers – suffering AChEi exposure – whose symptoms ”mirror those” of GWI (1), implying a similar ‘mirroring’ with those of SBS.(3,4)
As quite potent AChEis are known to naturally occur in mold species associated with SBS, (5,6,7) there indeed appears to be a common denominator to explain the stated similarities of the symptoms/maladies in question. Of course, beyond the fact of such similarities, a question is highlighted as to what the full public health impact of AChEi exposures may be, what maladies such exposures – in fact – may be the cause of.
GWI, AChEis, and SBS
”Each of the major types of AChEi exposure that GWV (Gulf War Veterans) experienced…is linked epidemiologically to illness with remarkable consistency. A dose-response relationship is present”, (1) read the Spring 2008 findings published in the Proceedings of the National Academy of Sciences of the United States of America. Notably, the study emphasized that criteria widely accepted for the determination of causality based upon observational data, Hill’s causality criteria, had been “arguably satisfied”.(1)
Golomb noted that only Hill’s final criterion, that of specificity, was somewhat in question, Golomb highlighting that causal relationships – by their nature – “routinely violated” this demand that an “exposure be linked only to the outcome examined”, citing alcohol’s generation of multiple problematic outcomes (accidents, liver problems, neuropathy, cancer) to illustrate her argument.(1) Then, assuming the linkage between GWI and AChEis as firm, an extraordinary similarity between symptoms of GWI and those of SBS would seem to suggest the possibility of common biochemical processes in play within both complaints.
Examining this GWI/SBS similarity, according to the so-called Kansas definition of GWI, there must be ”multiple or at least moderately severe symptoms in three or more of six symptom groups, focused on fatigue/sleep, pain, neurological/cognitive/mood, gastrointestinal, respiratory, and skin problems.”(1) Providing a virtual ‘mirror image’, according to a 1997 study by Redlich, Sparer, and Cullen, symptoms of SBS include: ”mucus-membrane irritation – eye irritation, throat irritation, cough; neurotoxic effects – headaches, fatigue, lack of concentration; respiratory symptoms – shortness of breath, cough, wheeze; skin symptoms – rash, pruritus, dryness; chemosensory changes – enhanced or abnormal odour perception, visual disturbances”.(3) In 1988, the World Health Organization listed similar symptoms, but also included ”gastrointestinal complaints”.(4)
_____

Does a common denominator of AChEi exposure explain such mirror imagery?
Again, potent AChEis emanate from particular groups of fungi often associated with incidents of SBS, or more specifically, from particular mycotoxins within these groups.(5,6,7) However, to date and in contrast to GWI, it appears research has yet to address the potential health effects this AChEi exposure may generate, the explanation for SBS it may provide.
We believe the SBS question may well be associated with mycotoxins such as Territrem B (TRB), ”a potent and irreversible inhibitor of acetylcholinesterase (AChE)”,(5) and one which has been found to exist in both Penicillium sp FO-4259 (6) and Aspergillus terreus.(5) This is particularly significant given that both Penicillium and Aspergillus are commonly associated with SBS,(7) though questions remain as to how broadly AChEis generally, and mycotoxins such as TRB particularly, may be found within each genus, as well as within other indoor molds.
Further, should the linkage we hypothesize between SBS and mycotoxin borne AChEis be proven, this is again not to say that other causes of SBS do not exist, for we believe they do (chemical pollutants). However, it is known that Penicillium sp FO-4259 contains multiple AChEis, including Arisugacins A and B, plus Territrems B and C, with the table immediately below highlighting their respective potencies.(6)

Low-Level Exposure and Chronic Symptoms
Questions regarding the impact of repeated low-level exposures to potentially toxic agents exist within the circumstances of both GWI and SBS. For GWI, ”evidence of chronic and delayed consequences to physiological systems from repeated low-level AChEi exposure” was found, with it being added that ”evidence for persistent and delayed effects of low-level exposure is accruing”.(1)
Paralleling the chronic nature of GWI, in 2004 it was observed that ”there is mounting evidence that some SBS symptoms do not abate quickly if at all”.(7) These researchers then immediately proceeded to note that ”evidence by numerous investigations has shown the association of various species of fungi including Penicillium sp and Aspergillus sp and their spores with indoor air quality problems and SBS”,(7) emphasizing the role these two fungi play.
Completing the evidence in this area were findings published Summer 2008 in what is believed to be the first ever ”follow-up study of patients previously referred to hospital” with “non-specific building-related symptoms”, SBS.(8) The study followed the experience of approximately 200 such patients who had indeed received hospital clinic treatment, observing that:
The level and severity of symptoms decreased over time, although nearly half of the patients claimed that symptoms were more or less unchanged after 7 years or more, despite actions taken. Twenty-five percent of the patients were on the sick-list, and 20% drew disability pension due to persistent symptoms at follow-up.(8)
The study also found that only about 7% of those patients followed had fully recovered from SBS’s effects.(8)
Evidence would seem to exist that repeated low-level exposures, in cases of both GWI and SBS, do appear to yield chronic and delayed consequences to physiological systems. It is unfortunate though that the phrase ’low-level’ can be somewhat misleading.
500-Fold Larger Exposures and Aerosolized Fungal Fragments
Examining the question of AChEi exposure via the inhalation of aerosolized fungal agents, 2002 research demonstrated that Aspergillus versicolor and Pencillium melinii fungal fragments were found to be “aerosolized simultaneously with spores from contaminated agar and ceiling tile surfaces.”(9) The study emphasized that the “considerable immunological reactivity, the high number, and the small particle size of the fungal fragments may contribute to human health effects that have been detected in buildings with mold problems but had no scientific explanation until now.”(9)
Mold fragments, not simply the spores, are thus suggested as harboring the potential to provide a key AChEi delivery mechanism. Subsequent research further highlighted an extremely significant role for fungal fragments, one as the primary medium for mycotoxin exposure from indoor-molds.(10) Specifically, a 2007 Swedish research study found, “indoor-molds may fragment into very small airborne mycotoxin-containing particles resulting in up to a 500-fold larger exposure than assumed previously.”(10)
Coupling the 2007 study’s findings with those from the independent 2002 research, a possible delivery mechanism for mycotoxins – and potentially AChEis – at levels hundreds of times higher than previously realized, would indeed seem suggested.
“Why are some ill and not others?”
Exploring beyond the possible role of AChEis in mold-related SBS, beyond the question as to how AChEi exposure might occur, the question of individual sensitivity to an AChEi exposure is raised. Given that we are addressing an onset of symptoms resulting from extended ‘low-level’ exposures, a question regarding the effects of individual differences in AChEi detoxification levels exists. We feel that the efforts of several studies are significant to cite in regards to this, with their findings of genetic variants noteworthy.
Returning to the findings published in the Spring 2008 Proceedings of the National Academy of Sciences of the United States of America , of particular significance is the determination that GWV illness was “linked to lower activity of AChEi detoxifying enzymes and genotypes conferring less-avid AChEi detoxification.”(1) The study noted that “low PON activity levels and concentration are significantly associated with multisymptom health problems in GWV”, singling out low PON1 activity for emphasis.(1)
Supporting such genetic linkage, a 1999 study’s title suffices: “Association of Low PON1 Type Q (Type A) Arylesterase Activity with Neurologic Symptom Complexes in Gulf War Veterans”.(11) An independent 2004 study also noted that their “finding parallels others’ observation of a link between PON1 heterozygosity” and symptoms in GWV.(12)
Paraoxonase (PON) is an enzyme which is HDL-associated, and “one of many circulating antioxidants thought to play a vital protective role”.(13) “The level of PON-1 gene expression is a major determinant of paraoxonase-1 status”, according to a 2003 French study.(14)
Evidence of a genetically based susceptibility to AChEi exposure appears to exist. Of course, the key question raised by this hypothesis is the impact mycotoxin derived AChEi exposures may have, particularly upon those most susceptible, and whether we have come to often term such impact SBS.
Conclusions
AChEi exposure, via inhaled AChEi-rich mycotoxins carried by aerosolized fungal agents, may be a primary but unrealized cause of SBS. Genetic variance, specifically involving low PON activity levels and concentrations, may be a key determinant of susceptibility to SBS. Research is needed to determine the answers to both these questions, as well as potentially that of how broadly, and in what configurations and potencies, AChEis may exist within the range of those fungi typically associated with SBS problems – Penicillium sp, Aspergillus sp, and Stachybotrys sp.
Potential Path for Research
The path forward is fairly simple, though the execution of it is not. A statistically significant sample of SBS sufferers would be secured, sufferers whose environment had remained essentially unaltered from the point of their symptoms’ onset, and where the environmental factors suggested the presence of mold (ie, dampness). An AChEi ‘inventory’ of each subject’s environment is then required, with a key factor in this being a complete environmental analysis to determine both the specific agents present, their concentrations, and their AChEi values. Testing the subjects to determine low PON activity levels and concentration would then further clarify the results. This PON testing would be particularly significant in cases where a number of individuals experienced similar exposures which resulted in markedly differing outcomes. A ‘control’ environment would also need to be ‘inventoried’, one where the environmental quality is known to be ‘high’. Then, pursuing an examination of the correlation between environmental AChEi levels and their components, individual PON levels, and subject outcomes, should highlight the validity of this paper’s hypothesis.
References
1. Golomb BA. Acetylcholinesterase inhibitors and Gulf War illnesses. 2008, PNAS,
vol. 105 no. 11, 4295-4300
2. Research Advisory Committee on Gulf War Veterans’ Illnesses Gulf War
Illness and the Health of Gulf War Veterans. Research Advisory Committee on Gulf
War Veterans’ Illnesses Home. November 2008. http://www1.va.gov/RAC-GWVI/
3. Redlich CA, Sparer J, Cullen MR. Sick-building syndrome. Lancet 1997; 349: 1013-
16
4. World Health Organization Indoor Air Quality: Biological Contaminants, 4-9,
Report on a WHO Meeting, Rautavaara, 29 August-2 September 1988
5. Chen JW, Luo YL, Hwang MJ, Peng FC, Ling KH. Territrem B, a
tremorgenic mycotoxin that inhibits acetylcholinesterase with a noncovalent yet
irreversible binding mechanism. 1999 J Biol Chem Dec 3; 274(49):34916-23
6. Shiomi K, Tomoda H, Otoguro K, Omura S. Meroterpenoids with various
biological activities produced by fungi. 1999 Pure Appl. Chem., Vol. 71, No. 6, pp.
1059-1064
7. Schwab CJ, Straus DC. The roles of Penicillium and Aspergillus in sick
building syndrome. Adv Appl Microbiol 2004; 55:215-38
8. Edvardsson B, Stenberg B, Bergdahl J, Eriksson N, Lindén G, Widman L.
Medical and social prognosis of non-specific building-related symptoms (Sick
Building Syndrome): a follow-up study of patients previously referred to hospital.
Int Arch Occup Environ Health 2008 Jul; 81(7):805-12
9. Górny RL, Reponen T, Willeke K, Schmechel D, Robine E, Boissier M,
Grinshpun S. Fungal Fragments as Indoor Air Biocontaminants. Appl Environ
Microbiol. 2002 July; 68(7): 3522-3531
10. Bloom E, Bal K, Nyman E, Must A, Larsson L. Mass Spectrometry-Based
Strategy for Direct Detection and Quantification of Some Mycotoxins Produced
by Stachybotrys and Aspergillus spp. in Indoor Environments. Appl Environ
Microbiol. 2007 July; p. 4211-4217, Vol. 73, No. 13
11. Haley RW, Billecke S, La Du BN. Association of Low PON1 Type Q
(Type A) Arylesterase Activity with Neurologic Symptom Complexes in Gulf War
Veterans. Toxicol Appl Pharmacol 1999 Jun 15;157(3):227-33.
12. McKeown-Eyssen G, Baines C, Cole DEC, Riley N, Tyndale RF, Marshall L,
Jazmaji V. Case-control study of genotypes in multiple chemical
sensitivity: CYP2D6, NAT1, NAT2, PON1, PON2 and MTHFR. Int J Epidemiol
2004 Oct;33(5):971-8.
13. Rainwater DL, Mahaney MC, Wang XL, Rogers J, Cox LA, Vandeberg JL
Determinants of variation in serum paraoxonase enzyme activity in baboons. 2005
Jul;46(7):1450-6. Epub 2005 Apr 16.
14. Gouédard C, Koum-Besson N, Barouki R, Morel Y. Opposite regulation of the
human paraoxonase-1 gene PON-1 by fenofibrate and statins. Mol Pharmacol,
2003 Apr;63(4):945-56.
//